Pelvic Floor Therapy
Vulvodynia

Ever felt that inexplicable, burning discomfort that just won’t quit? Vulvodynia, a term that might sound like a complex medical enigma, can feel that way. It’s that persistent vulvar pain that sneaks into intimate moments, daily routines, and even your workout sessions, making you wonder if your pelvic floor and overall well-being are secretly staging a rebellion. But don’t worry; we’re here to break it down, serve you the latest on pelvic floor exercises, pelvic floor health, pelvic floor therapy, and a whole lot more with a fresh, Gen-Z and millennial-friendly twist.
Quick Links to Useful Sections
- Understanding Vulvodynia: What’s Going On Down There?
- Symptoms, Diagnosis, and the Real-Life Impact
- Exploring Treatment Options: From Medical Therapies to Home Remedies
- Conventional Medical Treatments
- Emerging and Complementary Therapies
- Vulvodynia and Your Pelvic Floor: An Intricate Connection
- Pelvic Floor Exercises: Empowering You to Take Control
- 1. The Gentle Kegel
- 2. Reverse Kegels
- 3. Integrative Core Work
- Holistic Approaches: Beyond the Physical
- Nutrition and Lifestyle: Fuelling Your Healing Journey
- Real-Life Stories: Empowerment Amidst the Challenge
- Resources and Community Support: Your Next Steps
- Building Your Personalized Pelvic Floor Therapy Plan for Vulvodynia
- Step 1: A Thorough Evaluation
- Step 2: Set Goals That Resonate
- Step 3: Integrate Variations in Treatment
- Step 4: Build Consistency Into Your Routine
- Step 5: Monitor, Reflect, and Adjust
- Vulvodynia FAQs: Your Most Pressing Questions Answered
- Your Journey Towards Lasting Vulvar & Pelvic Health
Understanding Vulvodynia: What’s Going On Down There?
Vulvodynia, pronounced vul-vo-DY-nee-uh, is a chronic pain condition that affects the vulvar area without a clear identifiable cause. Unlike infections or obvious injuries, this condition tends to come with a mysterious flair, leaving many women (and some non-binary folks) searching for answers. It’s important to note that vulvodynia isn’t a disease but rather a symptom, often characterized by burning, stinging, irritation, or raw discomfort in the vulva.
At its core, vulvodynia can be likened to that annoying notification you never turned off, persistent, hard to ignore, and sometimes downright disruptive. Whether it flares up during daily routines or in moments of intimacy, its impact on pelvic floor health is undeniable. And while the reasons behind it can be as elusive as your Wi-Fi during a storm, researchers believe factors like nerve irritation, hormonal imbalances, and even muscle dysfunction play a role.
For anyone experiencing this condition, understanding vulvodynia is the first step in reclaiming your comfort and well-being with the help of pelvic floor therapy, supportive lifestyle changes, and targeted exercises.
Symptoms, Diagnosis, and the Real-Life Impact
Living with vulvodynia can feel like juggling a bunch of contradictory messages from your body. On one hand, there's a burning, stinging sensation that pops up without warning, and on the other, moments when even sitting for too long becomes a challenge. Here’s a quick rundown of what you might experience:
- Chronic Vulvar Pain: This isn’t your average discomfort but a persistent pain that may feel like a deep, burning inferno in the vulvar region.
- Irritation and Sensitivity: Everyday activities like showering, using certain fabrics, or even cycling can trigger flare-ups.
- Dyspareunia: Pain during intercourse, which can lead to stress, anxiety, and a noticeable impact on your intimate relationships.
- Emotional Toll: The ongoing discomfort can affect self-esteem, mood, and overall quality of life.
Getting a diagnosis for vulvodynia isn’t always straightforward. Since its symptoms can mimic other conditions, healthcare providers typically rule out infections, dermatological issues, and other disorders before confirming a vulvodynia diagnosis. This often involves pelvic examinations, lab tests, and sometimes even referral to a pelvic floor physical therapist.
The impact of vulvodynia goes far beyond physical discomfort. It affects mental health, intimate relationships, and overall quality of life. Recognizing these connections has led many to explore comprehensive treatment plans that combine pelvic floor therapy, exercises, and even holistic approaches.
Exploring Treatment Options: From Medical Therapies to Home Remedies
When facing vulvodynia, the treatment landscape can seem like a sprawling maze, but there’s a wealth of options designed to address this condition from multiple angles. Whether you’re drawn to conventional medical approaches or intrigued by holistic remedies, understanding your treatment options is key to reclaiming your pelvic floor health.
Conventional Medical Treatments
The cornerstone of treating vulvodynia often lies in conventional medical treatments:
- Topical Medications: Doctors may prescribe creams or gels, sometimes laced with anesthetics or anti-inflammatory agents, to reduce pain and irritation.
- Oral Medications: Neuromodulators or antidepressants may be recommended by some healthcare providers to help manage chronic pain symptoms.
- Pelvic Floor Physical Therapy: A specialized therapist can assess and treat any underlying muscle dysfunction. Targeted pelvic floor exercises not only strengthen the muscles but also improve coordination and reduce dysfunctional tension that may exacerbate vulvodynia.
- Injections: In some cases, nerve blocks or injections of medications like Botox may be employed to alleviate severe muscle spasms in the pelvic region.
While these treatments may require a bit of trial and error to pinpoint the most effective solution, they offer a robust starting point in calming the storm of vulvar discomfort.
Emerging and Complementary Therapies
Beyond the creased pages of your doctor’s prescription pad, complementary therapies are gaining traction as part of a holistic approach:
- Acupuncture: With roots deep in ancient wisdom, acupuncture is believed to help mitigate nerve pain and reduce inflammation by stimulating specific points along the body’s energy pathways.
- Massage and Myofascial Release: Gentle massage techniques can help release tightness in the pelvic and surrounding muscles, potentially reducing pain and improving overall pelvic floor health.
- Biofeedback: Using technology to monitor muscle activity, biofeedback can train you to relax or contract the right muscles at the right time, making pelvic floor exercises more effective.
- Cognitive Behavioral Therapy (CBT): Because chronic pain can take a toll on mental health, CBT can help you develop coping strategies and reshape the way you perceive pain, reducing its emotional impact.
The key is to craft a multifaceted treatment plan that aligns with your specific struggle with vulvodynia, ultimately intertwining professional guidance with home-based practices.
Vulvodynia and Your Pelvic Floor: An Intricate Connection
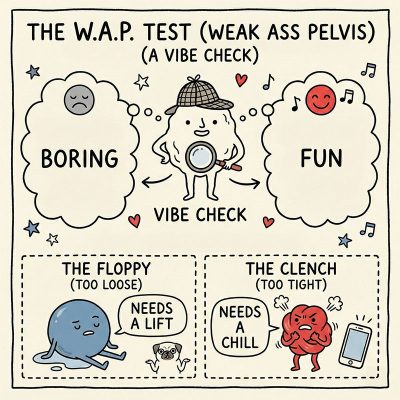
What do your pelvic floor, pelvic floor exercises, and vulvodynia have in common? A whole lot more than you might think. The pelvic floor is a complex web of muscles, nerves, and connective tissue that supports the bladder, bowel, and, yes, the vulva. When those muscles are too tense, too relaxed, or misfiring, the result can be chronic pain, discomfort, and other dysfunctions.
For many women experiencing vulvodynia, the pelvic floor itself can become a source of the problem. Muscle spasms or hypertonicity, where the muscles remain in a constant state of contraction, can heighten sensitivity and even exacerbate pain during daily activities and intimate moments. This is where targeted pelvic floor therapy comes into play.
Engaging in pelvic floor exercises that emphasize both relaxation and strengthening can break the cycle of chronic tension. Whether you’re trying to soothe tense muscles through reverse Kegels or build supportive strength through coordinated contractions, a trained pelvic floor therapist can help tailor these exercises to mitigate vulvar pain.
Pelvic Floor Exercises: Empowering You to Take Control
Let’s get real, navigating pelvic floor exercises can feel daunting, especially when vulvodynia is throwing your day off balance. But once you unlock these techniques, you’re not just exercising; you’re actively reclaiming control over your body. Here are some must-try movements that can alleviate discomfort and enhance pelvic floor health:
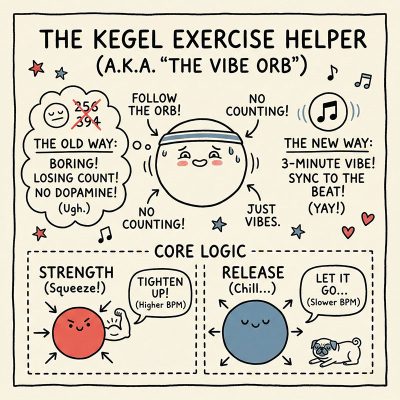
1. The Gentle Kegel
Often suggested as a go-to move, Kegels target the muscles responsible for bladder control. But when dealing with vulvodynia, it’s critical to perform them correctly. Start slow, contract your pelvic muscles gently, hold for a few seconds, and then relax. The trick is to avoid clenching too hard; think of it as giving your inner muscles a friendly nudge rather than an intense workout.
2. Reverse Kegels
These exercises focus on releasing tension rather than tightening up. Instead of contracting, you allow the muscles to relax fully, which can help alleviate hypertonicity that’s often linked with vulvodynia. Try to combine deep, relaxed breathing with these movements to create a calming routine.
3. Integrative Core Work
Incorporating pelvic floor exercises with core-strengthening moves, such as Pilates or yoga poses (hello, bridge pose and pelvic tilts!), enhances overall stability. The synchronization between core stability and pelvic muscle control not only improves pelvic floor health but also helps you feel more centered.
Remember, consistency is key. Whether you’re using smartphone apps for guided routines or attending sessions with a specialized pelvic floor therapist, gradual daily practice can transform your comfort level over time.
Holistic Approaches: Beyond the Physical
Managing vulvodynia isn’t just about treating the pain in your vulva, it’s about nurturing your entire self. Integrating holistic methods with conventional pelvic floor therapy brings together physical, mental, and even spiritual elements for a well-rounded approach to healing.
For instance, mindfulness meditation and deep breathing exercises aren’t just trendy relaxation hacks; they have a real impact on how your body processes pain signals. When you’re relaxed, your muscles, including those in your pelvic floor, are more likely to let go of chronic tension. Add to that a balanced anti-inflammatory diet and regular physical activity, and you have a potent mix of strategies to combat vulvodynia from all sides.
Yoga and Pilates classes tailored for pelvic floor health have surged in popularity, and it’s not hard to see why. They combine flexibility, strength training, and breath control, all of which help in reducing pain and improving overall pelvic function. Just as self-care has become a mantra in the modern age, these holistic practices encourage a deep, mindful connection between you and your body, ideal for managing vulvar pain.
Nutrition and Lifestyle: Fuelling Your Healing Journey
What you eat can either fan the flames of inflammation or help extinguish them. An anti-inflammatory diet is not just a buzzword, it’s a cornerstone for managing conditions like vulvodynia. Imagine your meals as a chance to soothe your body's inner battleground.
Focus on foods rich in omega-3 fatty acids, antioxidants, and fiber. Think salmon, walnuts, leafy greens, berries, and whole grains. These superfoods help reduce inflammation and promote tissue repair. At the same time, cutting down on highly processed foods, sugar, and excessive caffeine can make a significant difference in reducing chronic pain flare-ups.
Hydration is equally essential. Drinking enough water throughout the day keeps tissues supple and supports overall muscle function, including those in your pelvic floor. And while we’re on lifestyle tips, let’s not forget stress management. Chronic stress can lead to heightened muscle tension; incorporating activities like journaling, creative hobbies, or even a late-night Netflix binge (in moderation) can work wonders for your mental health.
Combine these nutritional and lifestyle shifts with your regular pelvic floor exercises and therapy sessions, and you create a holistic support system that can turn your healing journey into a truly empowering experience.
Real-Life Stories: Empowerment Amidst the Challenge
Nothing speaks louder than real-life transformation stories. Meet Jasmine, a 29-year-old creative professional, who battled chronic vulvar pain for years. After a diagnosis of vulvodynia left her questioning intimacy and self-care routines, Jasmine discovered the power of an integrative approach. Combining pelvic floor physical therapy with reverse Kegels and mindfulness-based stress reduction techniques, she gradually transformed how she experienced her body. Over time, her discomfort lessened, and she found a renewed confidence in both her health and her relationships.
Then there’s Elena, a fitness enthusiast who didn’t let vulvodynia sideline her passions. With a blend of specialized pelvic floor exercises, core stability workouts, and an anti-inflammatory diet, Elena learned to listen to her body’s cues and adjust her routines accordingly. Her journey is a testament to the idea that when you approach your pelvic floor health holistically, healing becomes a dynamic process, one that encompasses both physical strength and emotional resilience.
These stories aren’t just inspirational tales; they are practical blueprints showing how a tailored mix of pelvic floor therapy, lifestyle adjustments, and a little bit of self-love can lead to profound improvements in quality of life.
Resources and Community Support: Your Next Steps
Healing from vulvodynia is not a solitary journey. As you delve into pelvic floor therapy and explore targeted exercises, remember that there’s a vibrant community out there ready to offer support, share insights, and celebrate progress. Whether it’s online forums, local support groups, or one-on-one sessions with pelvic floor specialists, connecting with others who understand your struggles can make all the difference.
Here are some actionable steps to bolster your healing process:
- Research and Book an Appointment: Start by finding a pelvic floor specialist who understands vulvodynia. Many experts offer telehealth consultations, making it easier than ever to get professional guidance.
- Join a Support Community: Look for online groups or local meetups where people share their vulvodynia journeys. Sometimes, knowing you’re not alone is the first step toward empowerment.
- Explore Trusted Resources: Websites of reputable organizations dedicated to women’s health are treasure troves of information on the latest research, pelvic floor exercises, and holistic therapies for vulvodynia.
- Create a Daily Wellness Journal: Document your symptoms, routines, moods, and triggers. Tracking your progress can offer valuable insights into which interventions work best for you.
- Advocate for Your Health: Do not hesitate to ask questions, seek second opinions, and push for treatment plans that consider the whole you, mind, body, and spirit.
Taking control of your healing journey means embracing both professional guidance and community support. It’s about being proactive, staying informed, and remembering that every step, no matter how small, brings you closer to a life free of persistent pain.
Building Your Personalized Pelvic Floor Therapy Plan for Vulvodynia
Crafting a treatment plan for vulvodynia is an art as much as it is a science. The ultimate goal? To create a synergy between targeted pelvic floor exercises, holistic practices, and lifestyle adjustments that help you reclaim comfort and confidence. Here’s how to start:
Step 1: A Thorough Evaluation
Engage with a specialist who understands that vulvodynia involves multiple dimensions, physical pain, emotional stress, and even hormonal factors. A comprehensive assessment not only examines your pelvic floor muscles but also considers your lifestyle, diet, and mental well-being.
Step 2: Set Goals That Resonate
Whether it’s reducing daily pain, regaining intimacy, or simply feeling more balanced, outline clear, achievable objectives. Your goals should inspire you and serve as benchmarks for progress as you navigate your therapy journey.
Step 3: Integrate Variations in Treatment
Combine the strengths of conventional pelvic floor therapy with complementary methods. This might include:
- Customized pelvic floor exercises, both strengthening moves like gentle Kegels and relaxation techniques like reverse Kegels.
- Complementary therapies such as acupuncture, massage, or even CBT to manage chronic pain and stress.
- Holistic practices like yoga, deep breathing exercises, and mindfulness meditation to promote a balanced mind-body connection.
- Nutritional guidance that supports tissue repair and reduces inflammation.
Step 4: Build Consistency Into Your Routine
Create a daily schedule that respects your body’s need for rest, movement, and mindful practices. Whether it’s dedicating 10 minutes to deep breathing before bed or a 20-minute gentle workout in the morning, consistency is your ally in achieving sustained relief.
Step 5: Monitor, Reflect, and Adjust
Keep an eye on how your body responds over weeks and months. Document your symptoms, mood changes, and any progress in a personal wellness journal. Regular check-ins with your healthcare provider will help you fine-tune your plan, ensuring that every element, from pelvic floor exercises to dietary tweaks, remains perfectly tailored to your evolving needs.
Remember, your personalized plan isn’t static. It’s a living document that grows and transforms with you, celebrating each improvement and recalibrating when challenges arise.
Vulvodynia FAQs: Your Most Pressing Questions Answered
We know that vulvodynia can feel overwhelming and confusing, which is why we’ve compiled some frequently asked questions to clear things up:
1. What exactly is vulvodynia?
Vulvodynia is a chronic pain condition characterized by burning, stinging, or irritation in the vulvar region without an identifiable cause. It’s not an infection but rather a symptom of various underlying factors including pelvic floor dysfunction and nerve sensitivity.
2. How is vulvodynia diagnosed?
Diagnosis typically involves ruling out infections and other conditions through pelvic exams, lab tests, and sometimes referrals to pelvic floor specialists. The process is about understanding the full picture of your pelvic health.
3. Can pelvic floor therapy help manage vulvodynia?
Yes, targeted pelvic floor therapy, including specialized exercises like Kegels and reverse Kegels, can help alleviate muscle tension and improve support in the pelvic region, which may reduce vulvar pain.
4. Are there holistic treatments that can complement medical therapies for vulvodynia?
Absolutely. Complementary therapies such as acupuncture, massage, mindfulness meditation, and nutritional adjustments can work hand in hand with conventional treatments to provide a more comprehensive approach.
5. How do I know which treatments are right for me?
A personalized evaluation by a vulvodynia specialist or pelvic floor therapist is key. They can help craft a treatment plan that considers your unique symptoms, lifestyle, and overall pelvic health.
6. Can lifestyle changes really make a difference?
Yes, lifestyle factors like stress management, a balanced anti-inflammatory diet, and regular gentle exercise can significantly impact both the physical symptoms and emotional toll of vulvodynia.
7. How long does it take to see improvements?
Every person’s journey is unique. While some may notice changes within weeks, others might take several months of consistent pelvic floor therapy and lifestyle adjustments to see significant improvements.
8. Is vulvodynia a lifelong condition?
The course of vulvodynia can vary. With the right mix of treatment, pelvic floor exercises, and holistic care, many individuals experience substantial relief and improved quality of life.
9. What role does mental health play in vulvodynia?
Mental health is integral to managing vulvodynia, as stress and anxiety can exacerbate pain. Mindfulness practices and cognitive therapies can be incredibly beneficial in alleviating the emotional burden.
10. Can I manage vulvodynia at home?
Many aspects of vulvodynia management, like pelvic floor exercises, mindfulness meditation, and dietary adjustments, can be implemented at home. However, professional guidance is recommended for tailored pelvic floor therapy and diagnosis.
Your Journey Towards Lasting Vulvar & Pelvic Health
Embracing the challenge of vulvodynia is about more than just managing pain, it’s about reclaiming your body, your confidence, and your freedom to live life on your own terms. With each pelvic floor exercise, mindful breath, and nutritional upgrade, you’re not just treating a symptom; you’re building an empowered future of pelvic health.
Picture a future where intimate moments aren’t hindered by discomfort and where your pelvic floor functions as a harmonious part of your overall well-being. Whether you are just beginning your journey or are well on your way to healing, every step you take is both courageous and transformative.
So, dive into pelvic floor exercises, experiment with complementary therapies, and don’t be afraid to ask for help. Your body is a living, breathing story of resilience and strength, and with the right blend of medical expertise, holistic practices, and community support, you can rewrite your narrative toward a life of comfort, balance, and joy.
Let every session of pelvic floor therapy and every moment of mindful relaxation be a tribute to your inner strength, one that says loud and clear: you deserve to own your health, embrace your body, and live your life to the fullest.
Curious About Your Pelvic Floor? Explore our curated collection of insightful articles to learn more and take charge of your health.
- Pelvic Floor Basics
- Pelvic Floor Exercises & Workouts
- Pelvic Floor Kegel Exercises: Techniques & Benefits
- Advanced Pelvic Floor Workouts
- Pre/Post-Natal Pelvic Floor Routines
- Pelvic Floor Exercises for Men
- Pelvic Floor Therapy Techniques
- At-home vs Professional Pelvic Floor Therapy Options
- Diet & Lifestyle for a Healthy Pelvic Floor
- Pelvic Floor Health & Wellness
- Specialized Pelvic Floor Conditions & Treatments
Now back to the main article!