Pelvic Floor Therapy
What Is Biofeedback For Urinary Incontinence?
Ever wondered how technology can help you take control of your pelvic floor, especially when urinary incontinence throws a wrench into your daily vibe? Biofeedback for urinary incontinence is like having a personal coach for your pelvic floor that whispers, “You got this!” in real-time, letting you see exactly which muscles are working (or not) during your pelvic floor exercises. Let’s dive into this high-tech, science-backed method that’s not only revolutionizing pelvic floor therapy but also bringing some serious empowerment to your wellness routine.
Quick Links to Useful Sections
- Understanding Biofeedback: The Modern Approach to Pelvic Floor Health
- The Science Behind Biofeedback for Urinary Incontinence
- How Does Biofeedback Therapy Work?
- Key Benefits of Using Biofeedback for Urinary Incontinence
- Combining Biofeedback with Pelvic Floor Exercises and Therapies
- Practical Tips and Step-by-Step Guide to Starting Biofeedback Therapy
- Step 1: Consult a Specialist
- Step 2: Get Acquainted with the Equipment
- Step 3: Learn the Fundamentals
- Step 4: Develop a Regular Routine
- Step 5: Monitor and Adjust
- Client Success Stories: Realizing the Benefits of Biofeedback
- Emma’s Journey: From Frustration to Empowerment
- Liam’s Recovery After Surgery
- Sophia’s Breakthrough: A New Lease on Life
- Addressing Common Concerns and Misconceptions
- Myth 1: Biofeedback is Invasive and Uncomfortable
- Myth 2: It’s Just Another Fad
- Myth 3: Only Women Benefit from Biofeedback
- Myth 4: Technology Can't Address Complex Health Issues
- Future Innovations in Biofeedback and Pelvic Health
- Resources and Community Support: Your Next Steps
- Frequently Asked Questions About Biofeedback For Urinary Incontinence
- Your Journey to Empowered Pelvic Health with Biofeedback
Understanding Biofeedback: The Modern Approach to Pelvic Floor Health
Biofeedback is a cutting-edge technique that uses electronic monitoring to translate the otherwise invisible activity of your pelvic floor muscles into understandable, visual, or auditory signals. For anyone dealing with urinary incontinence, this technology becomes a game-changer by providing precise feedback on muscle performance during exercises. In other words, you’re not just guessing if your pelvic floor is working correctly, you can actually see and feel what’s happening.
In our tech-savvy world, biofeedback bridges the gap between ancient pelvic floor exercises and modern innovation. Whether you’re new to pelvic floor therapy or a seasoned wellness enthusiast, biofeedback invites you to transform your approach to health by actively engaging with the process. With this intimate window into your body’s inner workings, managing urinary incontinence can be as satisfying as hitting the perfect beat on your favorite playlist.
The Science Behind Biofeedback for Urinary Incontinence
At its core, biofeedback is a physiological monitoring technique. Sensors are attached to your skin or inserted in a way that is comfortable, and they measure signals like muscle tension, contraction strength, and even nerve impulses. These signals are then converted into visual graphs, sounds, or even haptic feedback.
When it comes to urinary incontinence, biofeedback targets the pelvic floor muscles, an essential muscle group responsible for bladder control. When these muscles are weak or not properly coordinated, urinary leakage frequently occurs. By providing immediate, real-time data on muscle engagement during exercises such as Kegels, biofeedback helps you hone in on proper technique and avoid overexertion or incorrect muscle recruitment.
The science behind this technology is both robust and increasingly accessible. Research shows that biofeedback not only helps improve muscle strength but also enhances coordination and awareness, leading to significant advancements in managing incontinence symptoms. When combined with traditional pelvic floor therapy and lifestyle modifications, biofeedback serves as a vital tool in a comprehensive approach to pelvic health.
How Does Biofeedback Therapy Work?
Picture this: You’re in a comfortable setting, perhaps in your own living room or a dedicated pelvic therapy office. A small device attached to you picks up the subtle signals from your pelvic floor muscles and transforms them into easy-to-read data. Here’s how the process generally unfolds:
- Sensor Placement: Specialized sensors are placed close to or directly on your pelvic region. These sensors are non-invasive and designed to capture the electrical activity and contraction patterns of your muscles.
- Signal Conversion: The sensors send data to a monitor or mobile device. The information is then processed and displayed as real-time graphs, charts, or even sound frequencies, offering immediate feedback on your muscle contractions.
- Guided Exercises: Under the guidance of a pelvic floor therapist or using an intuitive mobile app, you perform targeted exercises while watching the live feedback. This visual or auditory cue helps you adjust your efforts to ensure you’re engaging the right muscles at the right time.
- Progress Tracking: Over time, the biofeedback system records your progress. By reviewing these trends, you and your healthcare provider can tailor your therapy sessions to enhance muscle strength and coordination even further.
Essentially, biofeedback transforms the abstract concept of “muscle awareness” into a tangible and measurable experience, making pelvic floor exercises more effective and engaging.
Key Benefits of Using Biofeedback for Urinary Incontinence
Biofeedback is not your average piece of gym equipment, it’s a smart, interactive tool that offers a variety of benefits for those dealing with urinary incontinence. Here’s why it has become a staple in modern pelvic floor therapy:
- Enhanced Muscle Awareness: With immediate data on your muscle activation, you build a deeper understanding of how your pelvic floor functions, making it easier to target and enhance those muscles.
- Precision Training: Biofeedback allows you to adjust and perfect your exercises with precision. By knowing exactly which muscles need extra work, your pelvic floor exercises become more tailored and effective.
- Motivational Boost: Seeing tangible progress in real-time can be highly motivating. It turns every exercise session into a mini achievement session, boosting your confidence and commitment to the process.
- Reduced Anxiety: Urinary incontinence can cause significant stress and self-consciousness. With biofeedback, you gain control and clarity about your body’s responses, thereby alleviating some of that anxiety.
- Customized Therapy: The data obtained allows therapists to design highly personalized treatment plans, ensuring that your therapy adapts as you progress.
- Resource Efficiency: By using technology to track progress, fewer unnecessary or ineffective exercises are performed, making your rehabilitation journey more time- and resource-efficient.
For anyone struggling with urinary incontinence, biofeedback isn’t just a technical gadget, it’s an empowering tool that translates the often-murky realm of muscles into clear, actionable insights.
Combining Biofeedback with Pelvic Floor Exercises and Therapies
While biofeedback on its own is revolutionary, its real magic happens when it’s intertwined with traditional pelvic floor exercises and complementary therapies. Think of it as the perfect duet where tech meets timeless exercise.
Many pelvic floor therapy programs now integrate biofeedback into their exercise routines, allowing for enhanced data-driven sessions that can be fine-tuned for better outcomes. Here’s how integrating biofeedback can add value to your routine:
- Complementary Kegel Training: Biofeedback provides clear indicators during Kegel exercises, ensuring you’re targeting the correct muscles. This is crucial because doing Kegels incorrectly can sometimes exacerbate issues rather than resolve them.
- Coordinated Routine Enhancements: Biofeedback works hand in hand with other pelvic floor exercises like reverse Kegels, core strengthening, and even yoga or Pilates moves that indirectly improve pelvic stability.
- Enhanced Recovery Programs: For individuals recovering from surgery, biofeedback coupled with guided exercises can dramatically improve outcomes, reducing recovery time and promoting proper healing.
- Holistic Health Integration: Beyond the physical, biofeedback ushers in a meditative quality into your exercise routine. Watching real-time metrics can become a form of mindfulness practice, helping to calm anxiety and reinforce a positive mind-body connection.
By synergistically blending modern biofeedback techniques with proven pelvic floor exercises, you not only educate your body but also set the stage for lasting improvements in urinary continence and overall pelvic health.
Practical Tips and Step-by-Step Guide to Starting Biofeedback Therapy
Ready to jump into biofeedback therapy and reclaim your pelvic prowess? Before diving in, consider these practical tips and a step-by-step guide that can help you transition from curiosity to confident action.
Step 1: Consult a Specialist
Start by consulting a pelvic floor therapist or specialist who has experience with biofeedback. They’ll assess your symptoms, explain the process, and determine if biofeedback is the right fit for your situation. A personalized evaluation is key to creating a treatment plan that’s as unique as you are.
Step 2: Get Acquainted with the Equipment
During an initial session, your therapist will explain how the biofeedback sensors work and where they’ll be placed. Don’t worry, these devices are designed to be comfortable and user-friendly. Consider it a high-tech peek inside your very own pelvic power plant.
Step 3: Learn the Fundamentals
With the sensors in place, your specialist will guide you through some baseline exercises. You’ll learn how to contract and relax your pelvic floor muscles, all while watching the real-time feedback on the monitor. This stage is all about building awareness and ensuring classic exercises like pelvic tilts, Kegels, and reverse Kegels are performed correctly.
Step 4: Develop a Regular Routine
Consistency is the name of the game. Schedule regular sessions, whether in-clinic or at home with mobile app support, to track your progress. The beauty of biofeedback is that it gives you measurable evidence of your improvement, turning each routine into a milestone on your journey to better pelvic health.
Step 5: Monitor and Adjust
As you progress, use the data from each session to fine-tune your exercises. Notice trends in muscle engagement, and don’t hesitate to discuss any concerns with your therapist. Adjustments may involve tweaking the intensity, frequency, or even the types of exercises you perform. This dynamic process ensures that your therapy plan evolves with your needs.
With these steps, you’re well on your way to mastering your pelvic floor like a seasoned pro. Embrace the journey, celebrate each small win, and remember: each contraction and relaxation is a step toward reclaiming control.
Client Success Stories: Realizing the Benefits of Biofeedback
Nothing speaks louder than real-life success stories. Across clinics worldwide, biofeedback therapy has transformed the lives of countless individuals battling urinary incontinence. Here are a few inspiring testimonials:
Emma’s Journey: From Frustration to Empowerment
Emma, a vibrant 28-year-old graphic designer, found that her busy lifestyle and constant stress were taking a toll on her pelvic health. After struggling with unpredictable urinary leakage, she turned to biofeedback therapy. With each session, Emma learned how to accurately contract her pelvic muscles. The progress was palpable, her biofeedback readings improved steadily, and for the first time in years, she felt in command of her body. “It wasn’t just the technology, it was the awareness and empowerment it brought,” Emma reflects.
Liam’s Recovery After Surgery
After undergoing surgery for a pelvic organ prolapse, Liam was determined to reclaim his strength. His recovery plan incorporated biofeedback-assisted pelvic floor exercises, which not only sped up his rehabilitation but also enhanced his posture and core stability. Liam’s recovery was so effective that he started recommending biofeedback therapy to friends and family who were facing similar issues. “Seeing the muscle activity in real time motivated me to stick with the program,” he shares.
Sophia’s Breakthrough: A New Lease on Life
For Sophia, a 35-year-old fitness coach, persistent incontinence was not only a physical challenge, but a blow to her self-confidence. After trying traditional pelvic floor exercises with limited success, she discovered biofeedback therapy. With guided sessions and real-time data, Sophia learned how to correct her technique and strengthen her pelvic floor. Over time, the improvements in her biofeedback results encouraged her to fully embrace the routine. Today, Sophia is not only in control of her symptoms but is also an advocate for biofeedback in fitness communities.
These stories illustrate that biofeedback therapy isn’t just a clinical procedure; it’s a recurring journey of empowerment, self-awareness, and personalized care. Each journey underscores the significance of combining modern technology with traditional therapeutic methods.
Addressing Common Concerns and Misconceptions
Despite its growing popularity, there are still some common concerns and misconceptions about biofeedback for urinary incontinence. Let’s debunk a few myths and clear up some frequently asked questions:
Myth 1: Biofeedback is Invasive and Uncomfortable
Many people worry that biofeedback might be uncomfortable or invasive. In reality, the sensors used in biofeedback are designed to be non-invasive and as comfortable as possible. Most patients compare the sensation to wearing a patch or a light band on the body, with minimal discomfort.
Myth 2: It’s Just Another Fad
While biofeedback might sound like a modern trend, it’s actually grounded in robust scientific research. Numerous studies have proven its effectiveness in improving pelvic floor function and managing urinary incontinence. When combined with traditional therapy, biofeedback has consistently shown positive outcomes.
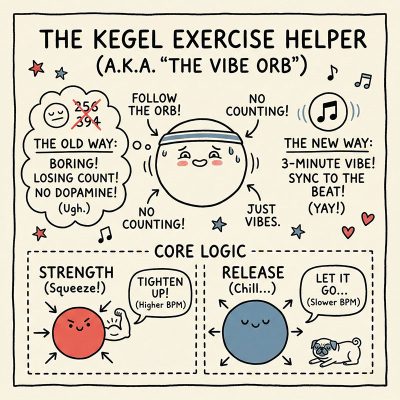
Ever wish your pelvic floor routine was as addictive as a video game?
Stop counting reps until you fall asleep and start feeling the rhythm. The Kegel Beat transforms a boring medical chore into a dopamine-fueled, 3-minute vibe.
Think of it as Guitar Hero for your pelvic floor. Just follow the pulsing Orb, sync your squeeze to the music, and lock in that strength without the snoozefest.
Ready to find your rhythm? Click here to play along.
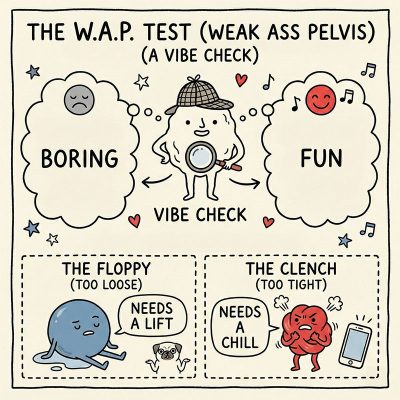
Is your undercarriage failing the vibe check?
It might be time to admit you have a W.A.P. (Weak Ass Pelvis). We replaced the awkward doctor’s visit with the ultimate "Pelvic Personality" quiz.
You start with a "Diamond Standard" score of 100%. But be warned: every sneeze-pee, jaw clench, and leak drains the tank.
Are you holding tension or barely holding it in? Click here to uncover your score.
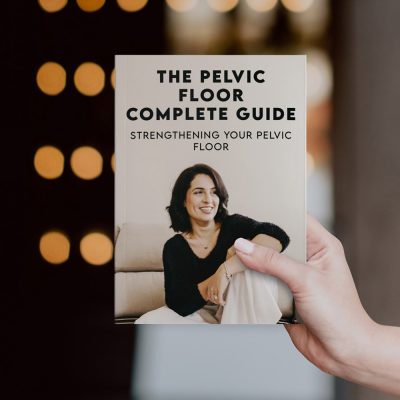
Do you secretly panic every time you feel a sneeze coming on?
Stop crossing your legs and start fixing the foundation. The Pelvic Floor Complete Guide is your no-nonsense roadmap to a bulletproof core.
We ditched the dry medical lectures for plain English, a killer 4-week routine, and the breathing hacks you need to stop leaks for good. Whether you're a new mum or a midlife warrior, get the strength to live leak-free.
Ready to be strong, not soggy? Grab the guide.
Myth 3: Only Women Benefit from Biofeedback
Although urinary incontinence is more commonly discussed among women, men can and do benefit from biofeedback therapy as well. Men facing post-prostate surgery rehabilitation, for example, often turn to biofeedback to rebuild their pelvic floor strength and reduce incontinence rates.
Myth 4: Technology Can't Address Complex Health Issues
It might seem counterintuitive that a piece of technology could address something as complex as muscle coordination and incontinence. However, biofeedback is less about the machine and more about providing you with actionable insights into your own physiology. Once you see the data, you can make real, informed decisions about your therapy.
Dispelling these myths is key to embracing biofeedback as a valuable ally in your journey to pelvic health. With real-time insights and personalized feedback, you’re better equipped to overcome urinary incontinence and restore confidence in your body’s abilities.
Future Innovations in Biofeedback and Pelvic Health
The field of biofeedback is evolving at a rapid pace, and future innovations promise to make pelvic floor therapy even more accessible and effective. Experts predict that the integration of artificial intelligence, machine learning, and wearable technology will push biofeedback to new heights. Imagine a wearable device that not only tracks your pelvic muscle activity but also analyzes your data to offer personalized exercise routines in real-time.
Upcoming advances might include:
- Enhanced Wearable Sensors: Lighter, more discreet sensors that provide even more accurate data, ideal for everyday use.
- AI-Driven Recommendations: Apps that leverage machine learning to analyze your biofeedback data and suggest modifications to your exercise routine on the fly.
- Virtual Reality Integration: Immersive VR experiences that guide you through pelvic floor exercises in an engaging, interactive environment.
- Remote Monitoring Solutions: Telehealth options that allow your therapist to track your progress in real-time from anywhere, ensuring that you’re always on the right track.
While the future is undoubtedly exciting, the current technologies already offer a transformative approach to managing urinary incontinence. As research continues to evolve, biofeedback will remain an essential component of modern pelvic floor therapy.
Resources and Community Support: Your Next Steps
Empowerment is at the heart of biofeedback therapy, and a well-supported community can make all the difference. As you consider incorporating biofeedback into your pelvic floor health routine, seek out local pelvic floor specialists, online support groups, and credible resources dedicated to pelvic wellness.
Some practical next steps include:
- Consult a Pelvic Health Specialist: Schedule an appointment to discuss your symptoms and learn if biofeedback is a fit for you.
- Join Online Communities: From social media groups to dedicated forums, connecting with others who share your experience can provide motivation and insights.
- Explore Mobile Apps: Several apps now integrate biofeedback data with guided pelvic floor exercises, offering an accessible way to stay on track.
- Educational Workshops: Look out for webinars and workshops hosted by experts to deepen your understanding of pelvic floor health and the latest treatment options.
When you combine personalized professional guidance with community support and readily available resources, you build a solid foundation for lasting change. This holistic approach to biofeedback and pelvic health ensures that you’re continually empowered, motivated, and informed.
Frequently Asked Questions About Biofeedback For Urinary Incontinence
The following FAQs address some of the most common questions we receive about biofeedback for urinary incontinence, providing you with clear, concise answers that blend science, practical advice, and a little bit of tech magic.
1. What exactly is biofeedback for urinary incontinence?
Biofeedback for urinary incontinence uses electronic sensors to monitor and convert the activity of your pelvic floor muscles into real-time feedback, allowing you to optimize your pelvic floor exercises and improve bladder control.
2. How will I feel during a biofeedback session?
Most patients find biofeedback sessions very comfortable. The sensors are non-invasive and designed for easy wear, and you might even appreciate how the immediate visual or auditory feedback enhances your exercise routine.
3. Can biofeedback help both men and women?
Absolutely. While urinary incontinence is often discussed in women, many men, especially those recovering from prostate surgery, benefit from biofeedback therapy to rebuild their pelvic floor strength.
4. What kinds of exercises will I perform during biofeedback therapy?
The sessions typically include targeted pelvic floor exercises such as Kegels, reverse Kegels, and core stabilization movements. The real-time feedback helps ensure that you’re engaging the correct muscles properly.
5. Is biofeedback a standalone treatment?
While biofeedback is highly effective, it works best when combined with a comprehensive pelvic floor therapy program that may include physical exercises, lifestyle adjustments, and sometimes complementary treatments like yoga or mindfulness.
6. How long does it take to see improvements?
The timeline varies for everyone, but with regular sessions, many patients begin to notice improvements within a few weeks to a couple of months. Consistency is key!
7. Are there any risks or side effects?
Biofeedback is considered very safe, with minimal risks. Most individuals do not experience any side effects, and any minor discomfort is temporary.
8. Can I use biofeedback at home?
Yes, many biofeedback systems are designed for home use. With guidance from your healthcare provider and a bit of practice, you can continue your therapy sessions with ease outside the clinic.
9. Do I need special equipment to get started?
Your therapist or a designated health professional will provide you with the appropriate equipment. There are also several consumer-grade devices available, although professional guidance is crucial for effective use.
10. How does biofeedback compare to traditional pelvic floor exercise methods?
Traditional exercises rely solely on self-awareness, which can be challenging without visual or sensory cues. Biofeedback enhances these exercises by providing real-time data, making it easier to identify incorrect techniques and progress more effectively.
Your Journey to Empowered Pelvic Health with Biofeedback
Embracing biofeedback for urinary incontinence is all about taking control. By combining cutting-edge technology with time-tested pelvic floor exercises and holistic lifestyle choices, you’re not just treating a symptom, you’re investing in a future of empowered, informed wellbeing. Every session, every contraction, and every visual cue on the monitor reinforces your growing mastery over your body.
Whether you're just starting out or have been on this journey for a while, remember that this technology is here to support you every step of the way. It’s about personalization, precision, and the relentless pursuit of a healthier, more confident you. With clear metrics, reproducible improvements, and a community of experts at your side, biofeedback empowers you with insights that go far beyond conventional exercise.
As you incorporate biofeedback into your pelvic health routine, embrace each small victory and learn to celebrate your progress, even on days when it feels like a marathon. With every guided exercise, you’re building a solid foundation for lasting control, confidence, and comfort. So, gear up, trust the process, and step confidently into a future where technology and wellness unite to create a harmonized, empowered pelvic floor.
Your journey to better pelvic health is not just about managing incontinence, it's about reclaiming your vibrant life, one breath, one contraction, and one moment of mindfulness at a time.
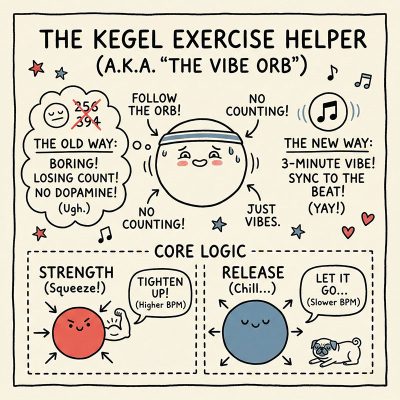
Ever wish your pelvic floor routine was as addictive as a video game?
Stop counting reps until you fall asleep and start feeling the rhythm. The Kegel Beat transforms a boring medical chore into a dopamine-fueled, 3-minute vibe.
Think of it as Guitar Hero for your pelvic floor. Just follow the pulsing Orb, sync your squeeze to the music, and lock in that strength without the snoozefest.
Ready to find your rhythm? Click here to play along.
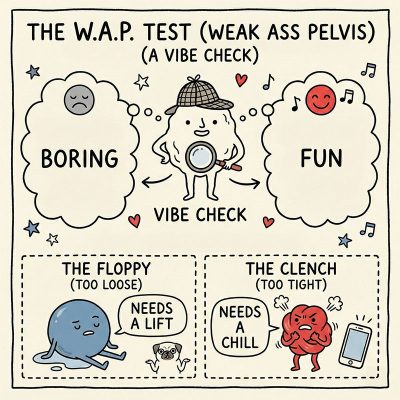
Is your undercarriage failing the vibe check?
It might be time to admit you have a W.A.P. (Weak Ass Pelvis). We replaced the awkward doctor’s visit with the ultimate "Pelvic Personality" quiz.
You start with a "Diamond Standard" score of 100%. But be warned: every sneeze-pee, jaw clench, and leak drains the tank.
Are you holding tension or barely holding it in? Click here to uncover your score.
Do you secretly panic every time you feel a sneeze coming on?
Stop crossing your legs and start fixing the foundation. The Pelvic Floor Complete Guide is your no-nonsense roadmap to a bulletproof core.
We ditched the dry medical lectures for plain English, a killer 4-week routine, and the breathing hacks you need to stop leaks for good. Whether you're a new mum or a midlife warrior, get the strength to live leak-free.
Ready to be strong, not soggy? Grab the guide.
Curious About Your Pelvic Floor? Explore our curated collection of insightful articles to learn more and take charge of your health.
- Pelvic Floor Basics
- Pelvic Floor Exercises & Workouts
- Pelvic Floor Kegel Exercises: Techniques & Benefits
- Advanced Pelvic Floor Workouts
- Pre/Post-Natal Pelvic Floor Routines
- Pelvic Floor Exercises for Men
- Pelvic Floor Therapy Techniques
- At-home vs Professional Pelvic Floor Therapy Options
- Diet & Lifestyle for a Healthy Pelvic Floor
- Pelvic Floor Health & Wellness
- Specialized Pelvic Floor Conditions & Treatments
Now back to the main article!